‘I’m so happy’: Nevada medical students find out residency match
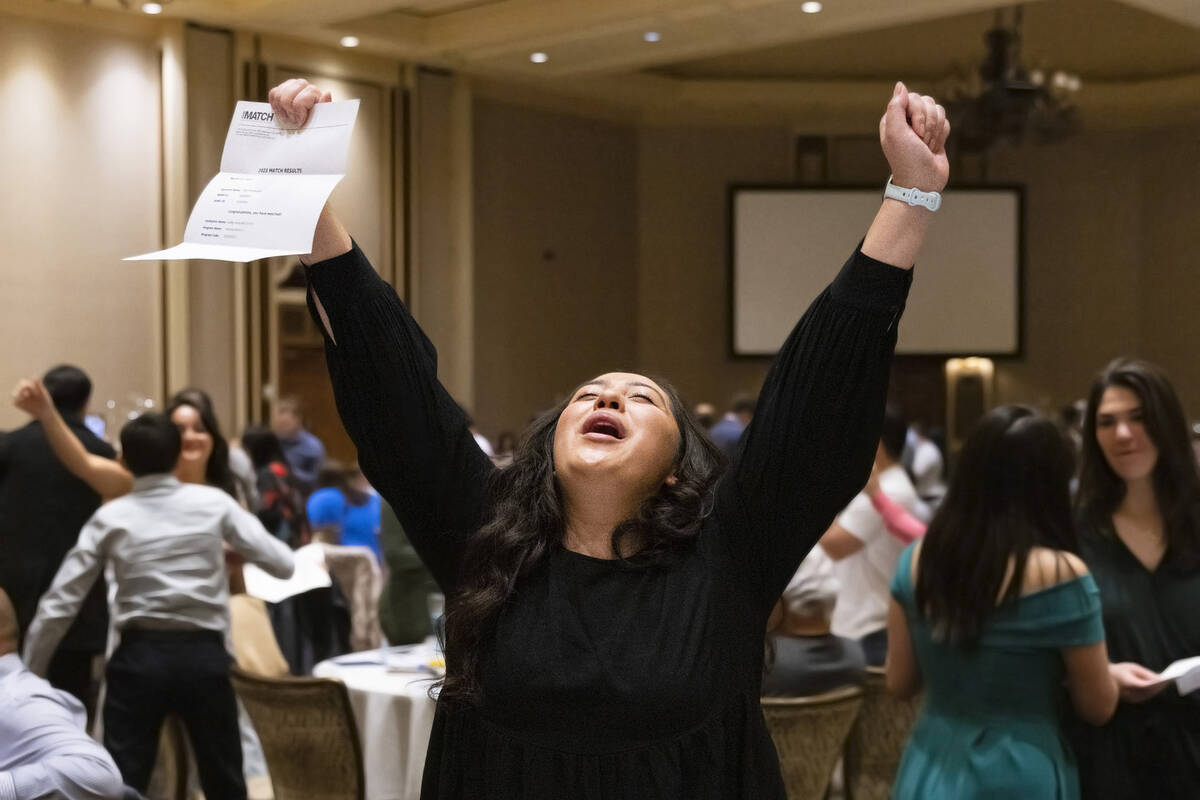
Touro University Nevada’s 160-plus graduating medical students each held a sealed envelope in their hands. Some of those hands were shaking.
“Rub it. Throw it in the air. Kiss it, whatever,” Dr. Wolfgang Gilliar, dean of the College of Osteopathic Medicine, said to the students assembled Friday morning in the grand ballroom of Green Valley Ranch Resort in Henderson.
The occasion? Match Day. This is when some 40,000 graduating medical students — nationwide and beyond — simultaneously open their envelopes at 9 a.m. Pacific Daylight Time to discover where in the U.S. they will be continuing their medical training as residents.
Just before 9 a.m., Gilliar asked the Touro students to observe a moment of silence to think about the physicians that they would become. Then it was go-time, with whoops of joy puncturing the silence.
“I’m so happy,” said Ellie Ok, who will be going to UCLA for a residency in physical medicine and rehabilitation.
“I’ve totally worked for this moment,” said Ok, a first-generation Korean-American who was the first in her family to go to college.
Match Day is the culmination of the National Resident Matching Program, which uses a mathematical algorithm to pair medical students with residency programs based on the ranked preferences of both. The algorithm was the basis for the award of the Nobel Prize in Economic Sciences in 2012.
Like Ok, Anjali Daulat brushed away tears of joy over her match with the University of Oklahoma-Tulsa, where she will be training in pediatric medicine.
“It’s such a feeling of relief. We’ve worked so hard for this,” Daulat said.
‘We have a brain drain’
Despite the evident joy, Match Day comes with a bittersweet note for leaders in medical education, who would like to see more graduates of Nevada’s medical schools stay within the state for their residencies. An in-state residency creates a greater likelihood that a physician will practice medicine in Nevada, where there is a shortage of doctors.
Part of the problem is that there aren’t enough spots in the state’s residency programs, Gilliar and Dr. Marc Kahn, dean of the Kirk Kerkorian School of Medicine at UNLV, said in interviews.
There also are no residency programs in Nevada for many specialties, including dermatology, urology and ophthalmology, Kahn said.
“Our students are going elsewhere in the country to do a residency in dermatology, and they’re not likely to come back,” he said. “What’s happening is we have a brain drain.”
Of UNLV’s 66 graduating medical students, 26 were matched with Nevada residency programs. Of Touro’s 162, 50 were matched in state.
In February, Kahn testified with UNR medical school dean Dr. Paul Hauptman before Nevada legislators about the need to increase state funding for residency programs.
Hauptman said that about half of Nevada’s medical school graduates eventually will practice medicine in the state. That proportion increases to roughly three-quarters if their residency training also is in the state, he said.
More residency spots would translate into more physicians in Nevada, which would result in more timely treatment and better outcomes, said Diego A. Trujillo, chief executive officer for Las Vegas HEALS, a health care association.
“All of this comes down to access to care,” he said in an interview.
Nevada is gradually increasing its number of residency positions.
This year, St. Rose Dominican will begin training its first-ever class of medical residents, a class of 12 for an internal residency program. Next year it will launch a second residency program, with a class of eight in family medicine.
St. Rose is focusing on primary care in its residency programs because the need there is so great, said Dr. Kimberly Bates, director of the internal medicine residency program.
“We’re missing that quarterback of the health care team because we don’t have enough primary care physicians,” she said.
The inaugural class of residents will be training at the St. Rose Dominican, St. Martin campus, and also at a neighborhood hospital at Martin Luther King Boulevard and Carey Avenue, a part of the community that is especially underserved.
Bates noted that much of Nevada has been federally designated as medically underserved, which she described as unusual. This creates an opportunity to have a great impact, she said, which is part of what drew her to Las Vegas from Georgia.
“That was the kicker for me.”
Spots in high demand
The UNLV medical school sponsors residency programs in 11 specialties and 11 fellowship programs in which residents and fellows provide supervised patient care at University Medical Center, its primary teaching hospital, as well as other locations in Southern Nevada.
The Sunrise Health System has residency programs in 10 different specialities ranging from diagnostic radiology to emergency medicine to neurology, said spokeswoman Jennifer McDonnell. Sunrise, MountainView and Southern Hills comprise the acute-care hospitals in the system.
The demand is high for these programs. For the anesthesiology residency program, there were more than 1,000 applications for eight positions, McDonnell said.
The Valley Health System, which has five acute-care hospitals, has three systemwide residency programs and four separate residency programs and two fellowship programs at Valley Hospital Medical Center, spokeswoman Gretchen Papez said.
Residency programs are primarily funded by the Centers for Medicare and Medicaid Services. Nevada has about 400 CMS-funded positions for all years of residency, compared with 9,000 in California and 16,000 in New York, Kahn said. The number of funded spots was essentially frozen in 1997; since then, Nevada’s population has more than doubled.
“It would be nice if the federal government relooked at the way they fund residency programs,” Kahn said.
The American Recovery Act created 1,000 new spots over five years, or 200 per year. “We were lucky to get two and a half of them in the first year,” he said. “In our opinion, myself and my colleague at UNR, we need to get the state to truly support GME (graduate medical education) if we’re going to fix our doctor shortage.”
A bill this legislative session proposes $8.5 million annually in residency funding for four years. Kahn and Hauptman are lobbying for at least double that. Funding also needs to be long term, the UNLV dean said.
It could take three years to establish a dermatology program and get it accredited, Kahn said. This means that four years of funding would pay for one-year of a residency, which, depending on the specialty, lasts between three and seven years.
“So we really need to get the state to buy into GME,” he said.
Contact Mary Hynes at mhynes@reviewjournal.com or 702-383-0336. Follow @MaryHynes1 on Twitter.