Ethiopian immigrant makes sure UMC rooms shine
There are soiled linens to bag, trash containers to empty, mirrors to clean, dusting to do, floors to mop, a toilet bowl to clean, disinfectant to apply.
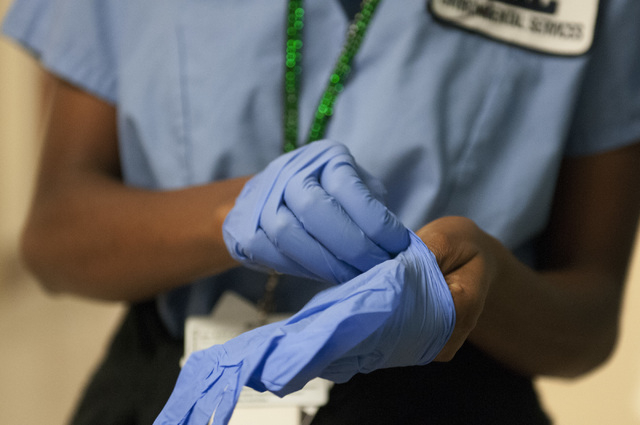
Disinfectant, or germicide, must be applied with a cloth to virtually everything, including the mattress, waste receptacles, light switches, call buttons, telephone, wall moldings, dispensers, windowsills and pieces of furniture (both inside and out). Floors are also mopped with an infection-killing cleaner.
Earlier in the day the patient in this University Medical Center hospital room was discharged and Seble Balcha, an environmental services aide, prepares it for the next visitor. During the half-hour she’s cleaning, she’s always moving: kneeling, pushing, pulling, rubbing, scrubbing, lifting, stretching — it’s all part of the job.
Soon, this woman, who was studying to be a lawyer in her native Ethiopia before she immigrated here four years ago, will be cleaning a bloody operating room.
“I see myself lucky,” she said before starting her workday, smiling as she struggled with the language she’s still learning at the College of Southern Nevada. “Because I was smart, the government in Ethiopia said I should be lawyer. I didn’t like, but I had no choice. Here, I have choice.
“I want to work one day in medical field as a respiratory therapist. That is my dream. But now, while I’m in school, I get a chance to learn about hospitals from the bottom up. To help people stay healthy — it’s a wonderful opportunity.”
The more time you spend with this 24-year-old immigrant, whose native language is Amharic, the more you realize just how important the work of an environmental service aide is.
And the more you realize why the United States, seen by many Americans as a place where only the well-off can have their dreams realized, remains a beacon of hope to people around the world.
“Sometimes,” said Lawrence Barnard, UMC’s chief operating officer, “it takes looking at things through an immigrant’s eyes to get a clearer picture of what this country offers, of how we should approach things.”
It is a Friday afternoon, about 45 minutes before Balcha’s night shift begins. She sits in the lobby of the trauma unit and explains how she got to this place in time. Largely raised by her grandfather who did well in the world of Ethiopian commerce, she said she already had a “nice life” there that provided her with “nice food,” “nice clothes” and “nice educational opportunities.”
Her future, she said, promised a lifetime of security had she become a lawyer as the government wanted.
“They needed lawyers and that’s what they thought I could be,” she said. “I was in my second year of law school when I came here.”
Just recalling that a government could force you into a particular occupation makes the smile on Balcha’s face disappear. “It is not right,” she said. “People must get the chance to make their own dreams come true.”
About five years ago in Ethiopia, Balcha was literally lucky — she was one of the yearly winners of the annual Diversity Immigrant Visa lottery run by the U.S. State Department, a program that saw her receive a U.S. permanent resident card, or green card. Last year, 55 million people applied worldwide, 55,000 won.
She came to Las Vegas because she said she had cousins and uncles here.
“It was a little bit hard for me to join with society at first,” she said, acknowledging that all the freedom “to do this or do that” was a little overwhelming.
She gave herself structure by taking English classes and by taking a variety of jobs while waiting for a job to open up in the health care field that she could do. She worked in a school dining room, with an electronics firm and in security at McCarran Airport.
“America is not easy,” said the woman who in 2010 won a beauty contest for Ethiopian immigrants in the United States. “You have to struggle by yourself to be someone. There is opportunity but it is hard work. People said I could be a good cocktail girl in a casino and make lots of money. But that wasn’t for me.”
No matter what job she had, Balcha said she worked hard at it.
“I had to show I was good worker and serious when I got a chance in health care,” she said. “You must take steps to get what you want in America. And I knew I wanted to help people in medical field. I had been around hospitals in my life. My dad and grandma were nurses.”
When an environmental services aide position opened up at UMC, she applied. Good references from her earlier jobs helped her get the job that pays $12.50 an hour. “I was so happy,” she said.
Although she didn’t see it as a career, she saw it as a crucial position within the hospital, and one that would allow her to see what position she’d like to pursue as a profession.
It didn’t take Balcha long to realize that an environmental services aide is the first line of defense in providing a safe patient environment and reducing hospital-associated infections. She said she does all she can to make sure that patient rooms and operating rooms are free of transmittable infection.
“Too many people in the United States get hospital infections,” she said. “I had thought that was only a problem in Africa. I feel sad. If everybody would do his own participation seriously, this would not happen. It’s a place where people should get healthy treatment. There are signs all over hospital to wash your hands, even in elevator. We must always remember that.”
Each year nearly 2 million hospital-acquired infections claim nearly 100,000 lives in the United States and add $45 billion in costs. The Institute of Medicine found that if hospital staff would make minor adjustments — such as washing hands more — the problem could be significantly reduced. A recent study out of England, where hospital infections are also prevalent, showed that a national campaign to increase hand hygiene cut the instances of MRSA (methicillin-resistant Staphylococcus aureus) and Clostridium difficile, commonly called C. difficile, two of the most common and deadly infections, by nearly 50 percent.
UMC has had some success in cutting infections. Its pediatric intensive care unit was one of only five such units nationwide to earn the Consumer Reports top rating for preventing bloodstream infections in 2012 — there were none. But overall the hospital earns average scores.
We’re studying how she (Dr. Meena Vohra) does it with her (pediatric) unit so we can duplicate it across the hospital,” UMC COO Barnard said.
One thing UMC is not doing, he said, is cutting the staff of environmental services aides. During the recent recession, the Association for the Healthcare Environment reported that many hospitals have cut environmental staff budgets by as much as 25 percent even as infection rates skyrocketed.
“It just makes no sense,” Barnard said.
Balcha’s doing her part to keep infections down. When supervisors inspect her work — a special black light picks up what is cleaned correctly — she earns 100 or 99.
“That’s not easy to do,” Operations Manager Linda Cox said.
One day, early on in her 18 months on the job, Balcha saw a respiratory therapist helping a person breathe.
“To do such a thing, helping people breathe, became my dream,” she said. She immediately signed up for CSN courses that would help pave her way into the therapist position.
That she wants to move up to a more skilled position impresses Barnard.
“There’s nothing I like more than to have an employee grow into another position,” he said.
Dawn Rooney, Balcha’s supervisor, calls her “an outstanding go-getter,” an employee who loves to greet people before she cleans their room.
“I make sure I put a smile on my face when I see a patient,” Balcha said. “I want them to feel good. I like talking with them.”
Dr. Dale Carrison, UMC’s chief of staff, said that few people, both inside and outside the hospital, give the environmental services aides credit for all they do: “You have to remember that what they do immediately cuts the risk of infection. And having a clean room is how many people judge a hospital. They get far too little thanks for what is tough work. Often all they hear is ‘do this and do that.’ Yet they’re good to our patients. They become the face of the hospital in patients’ rooms.”
Even though her work is applauded at UMC, Balcha acknowledged she wasn’t sure she could do it at first.
“I never had seen many bloods and bodily fluids,” she said. “But I’m getting used to it.”
On this day, the operating room she’s about to clean is bloody, but nowhere near as bloody as some she’s cleaned. Sometimes, she said, particularly in trauma, there will be blood on the ceiling, walls, everywhere.
Just as on this day, she said, other staffers show up to help out.
In less than an hour Balcha, Ronald Lacey and Veronica Nunez have the operating room sparkling.
No matter how busy the operating rooms become later on this night, Balcha said they will all be carefully cleaned with the best disinfectants.
“I care about people like I would want them to care about me.”
Contact reporter Paul Harasim at pharasim@reviewjournal.com or 702-387-2908.