Staff shortages, lack of beds bring hospitals closer to ‘breaking point’
Zachary Pritchett is feeling too exhausted to sleep.
The nurse’s back aches from turning ventilated patients onto their stomachs at his Henderson hospital. His feet are sore from working 12-hour shifts in the intensive care unit. When he goes home, he heads straight to bed, but his mind keeps turning.
Pritchett, 33, is thinking about how overworked his co-workers are. Some are seeking counseling, and one nurse could barely walk to her car this week after working 10 days straight.
The ICU is already full at the Siena campus of St. Rose Dominican Hospital, Pritchett said. As he lies in bed, he wonders when it will be too much.
“It’s not sustainable at all,” he said Thursday. “I would say we’re fast approaching our breaking point.”
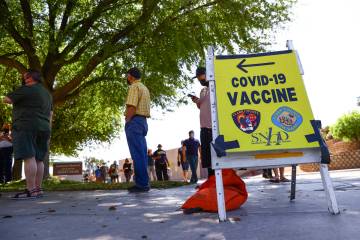
Frontline hospital workers in Clark County say the COVID-19 surge is pushing them to their limits despite the Nevada Hospital Association’s assurances that the region’s hospitals have room to take on more patients.
While hundreds of beds remain empty countywide, eight of the county’s 17 acute-care hospitals reported reaching or exceeding the maximum capacity of their staffed hospital beds for at least one day during the first half half of December. Thirteen reported the same for their staffed adult ICU beds, and eight reported a “critical staffing shortage,” according to NHA data obtained by the Review-Journal.
The surge in patients has prompted one hospital to hire more than 150 part-time workers to bolster its ranks since November.
The hospital association compiles hospital-level data daily but only shares aggregated county-level data with the public or most public health officials. The hospital-level data is provided to Nevada COVID-19 response director Caleb Cage, a member of Gov. Steve Sisolak’s office. The Review-Journal obtained copies of the reports spanning Nov. 2 through Dec. 15 using the state’s public records law.
Hospitals report both numbers of staffed and licensed beds. The former describes beds the hospital has sufficient staff on hand to care for, while the latter is the maximum number of beds the hospital is approved to have.
NHA officials refused to speak with the Review-Journal this week about the hospital-level data. Spokeswoman Amy Shogren said the association considers the information confidential despite regularly sharing it with the governor’s office.
During a Nevada COVID-19 Task Force meeting Thursday, association executive Chris Lake told government officials that hospitals statewide “have some challenges” with staffing and discharging recovering patients. But the association maintained as recently as Monday that Nevada’s health care infrastructure “remains intact and in fair condition,” even as COVID-19 hospitalizations have more than quadrupled since September, shattering records.
Sick, tired, overworked
Clark County hospital workers, however, say current patient loads are already overwhelming their facilities.
The labor and delivery unit at one of the Las Vegas Valley’s largest hospitals is housing overflow patients who don’t have COVID-19, nurse Yarleny Roa-Dugan said. ICU and emergency room staffers are working mandatory overtime shifts.
“They’re sick, they’re tired and they’re overworked,” said Roa-Dugan, who requested her employer not be named. “We don’t think we can keep going at this pace.”
At another major hospital, patients are being held in the emergency room because there’s not room for them elsewhere, emergency nurse Ralaya Allen said. She recently worked 14 days straight to help the hospital keep up with demand.
“Patients don’t stop coming, and with COVID, they’re sicker,” she said. “We’re already bursting at the seams.”
The same practice is happening at the Siena campus of St. Rose Dominican Hospital, Pritchett said. Some patients are waiting for days before being moved from the emergency department. The hospital’s standard nurse-to-patient ratios often cannot be met.
Despite this, Pritchett’s hospital did not report a critical staffing shortage in early December, according to the data obtained by the Review-Journal. The hospital also reported it was slightly under its capacity for staffed ICU beds most days and only reached its maximum capacity once.
The nurse said he vehemently disagreed with that assessment.
“The truth of the matter is that on the floor, we are short, and we are hurting for staff,” he said. “The nurses are spread so thin, they’re not able to spend quality time with their patients.”
A doctor with the Valley Health System in Las Vegas said the company is trying to acquire more nurses for its six acute-care hospitals, but a nationwide shortage is making it difficult to find any.
Southern California hospitals ran out of available intensive care unit beds on Thursday, and public health officials there say they are also facing staffing shortages.
“I think every hospital is competing for the same small group of nurses,” said the doctor, who spoke on condition of anonymity.
Discharging recovering COVID-19 patients is also becoming more difficult for Clark County hospitals, the NHA data shows. The number of medically cleared patients who were waiting to be discharged to a skilled nursing facility or other alternate care site rose from less than 20 in early November to 120 by mid-December.
Nevada health officials have formed a “hospital discharge strike team” to address the issue, state Department of Health and Human Services spokeswoman Shannon Litz wrote in an email. That includes weekly meetings with hospitals and skilled nursing facilities to help find placement for recovering patients.
“Each region within the state has dedicated staff assigned to work with on these issues,” Litz wrote.
“This is not a one-size-fits-all approach and we are building strategies to help facilities.”
Staffing critical during surge
Clark County has backup plans if local hospitals run out of space for patients.
The Las Vegas Convention Center could be turned into an alternative care site, adding hundreds of beds for patients with less serious injuries and ailments. But such a facility would need doctors, nurses and technicians to treat patients.
“It takes people to take care of other people,” University Medical Center CEO Mason Van Houweling said. “We couldn’t operate without them.”
UMC was among the hospitals that did not report a critical staffing or bed shortage in early December, but Van Houweling said it has required a “delicate balance” to keep the hospital appropriately manned. That includes not granting employees’ time-off requests for the holidays, having staff work an extra day per week and enrolling administrators to care for patients.
The hospital has also hired more than 150 part-time staff in the past six weeks. It’s a strategy many hospitals may not be able to afford now.
Increased demand nationwide for temporary nurses has led staffing agencies to effectively double their pay demands, Van Houweling said. Hospitals can expect to pay $7,000 per week for an ICU nurse, if they can find any to hire.
“At the current levels, it’s being managed,” he said of Southern Nevada’s COVID-19 surge. “(But if) hospitalizations go up … we could be edging into that staffing crisis.”
In Reno, Renown Regional Medical Center reported operating over capacity almost every day in early December. But it reported no critical staffing shortages.
As of Friday, the hospital was caring for 21 patients in an overflow medical unit that opened inside its parking garage last month. Almost 400 patients have been treated in the unit since it opened, the hospital reported.
Hospitals quiet about reports
Las Vegas hospital officials whose facilities reported staffing and occupancy shortages declined to be interviewed this week.
Valley Health System owns Henderson Hospital, which reported being critically short on staff every day from Dec. 1 through Dec. 15. Another one of the company’s facilities, Spring Valley Hospital, reported its ICU was full for 13 days in the same time frame.
Instead of an interview, Valley Health System spokeswoman Gretchen Papez wrote in a statement that her company was working to “free up ER and inpatient beds” and that “other areas of the hospital can be used to care for patients if needed.”
Sunrise Hospital, the largest in Southern Nevada, reported a critical staffing shortage for at least eight days straight this month. MountainView Hospital reported 10 days of shortages. Southern Hills Hospital operated with its ICU beds at maximum capacity, or over, for 14 days.
HCA Healthcare, owner of all three hospitals, also released a statement instead of having an official speak about the issues. Company spokesman Antonio Castelan wrote the hospitals were postponing elective surgeries to free up beds and “surging staff and ICU capacity, ensuring we are prepared to care for our patients and protect the health and well-being of our colleagues.”
St. Rose Dominican’s two hospitals with ICU units reported they were operating near or at capacity throughout early December. The system’s Las Vegas campus reported its staffing was critically short for eight days in a row.
Friday morning, Dignity Health-St. Rose Dominican Hospitals spokesman Gordon Absher said company officials were not available for an interview and were preparing a statement. As of Friday evening, it was not provided.
Pritchett said the lack of communication from hospital administrators has been felt by nurses at his job site.
“What are they hiding? That’s my question,” he said. “There are times when we can’t even get a response to our emails to administration.”
Contact Michael Scott Davidson at sdavidson@reviewjournal.com or 702-477-3861. Follow @davidsonlvrj on Twitter.