Coronavirus can isolate people with mental health issues
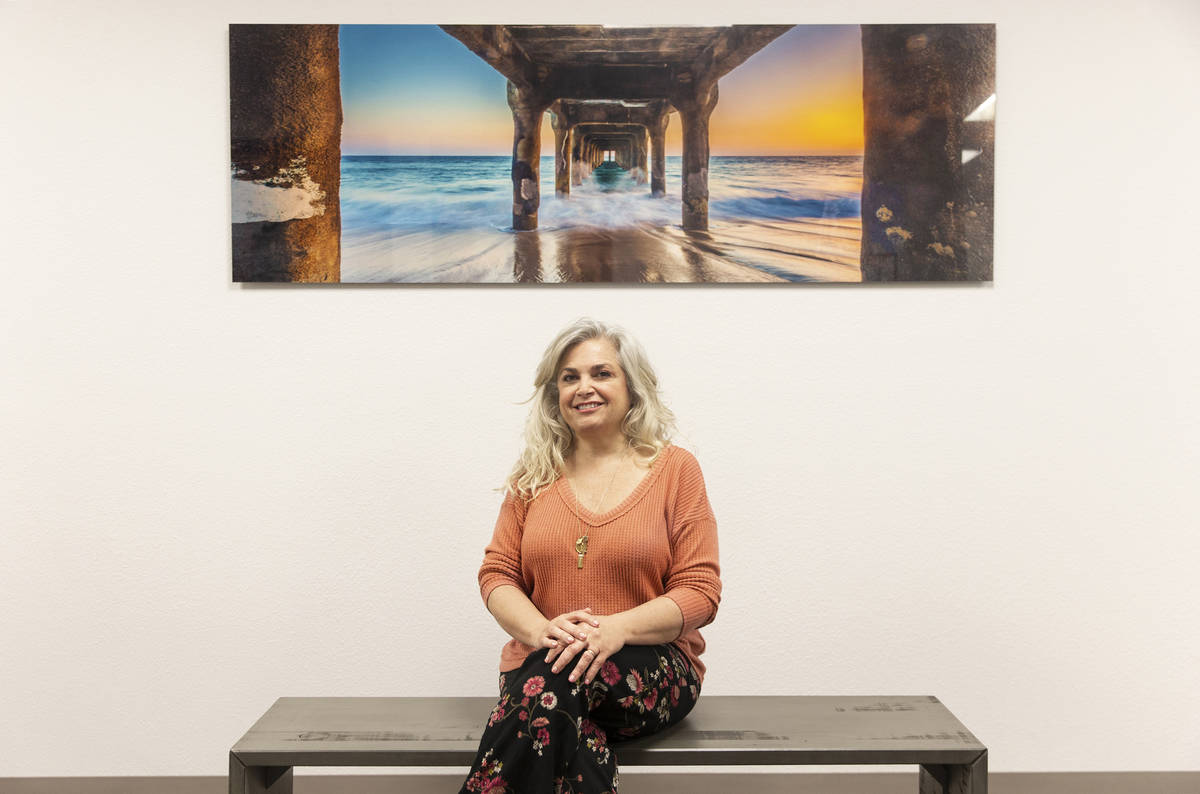
In the battle against inner demons, Alexis Gonzalez warred her way to a truce.
The business owner and dance instructor, who moved to Las Vegas with her mother in her late teens before relocating to Chicago two years ago, had gained control over her depression, anxiety and addiction, relying in no small part on group therapy.
Last month, she returned to Vegas to visit her mom while en route to India.
Then the coronavirus hit.
Social-distancing measures ended her in-person therapy sessions.
For Gonzalez, and others disinclined to discuss problems or whose mental health issues already involve isolating, that is no small thing.
“This situation is perfect to feed on our insecurities and develop our monologue inside our head because we’re not in contact with other people,” says the 31-year-old.
The support system that she and so many others rely on for mental health treatment was turned on its head almost overnight.
“An entire system (had) to dramatically change the way service is delivered,” says Dr. Jonathan G. Still, a Las Vegas psychiatrist and partner in Focus Mental Health Solutions. “Clinics and clinical entities that weren’t set up to engage patients at home are at a real disadvantage. It’s made our patients very, very isolated.
“There just aren’t enough psychiatrists in town,” says Theresa Noonan, a marriage and family therapist who owns Noonan Psychotherapy in Las Vegas. “The waiting lists are ridiculous.”
According to a 2019 report from the State of Nevada’s Commission on Behavioral Health, Nevada ranks 44th out of 50 states in prevalence of mental illness; 47th in access to care; 32nd in size of mental health workforce; and last in the number of youth suffering from major depression.
While the need for mental health care is high, Nevada’s ability to provide it remains low.
“We’re really struggling with fewer and fewer mental health resources in the community as providers are closing up shop because they haven’t adopted telehealth,” Still says. “It’s put a stress on a system that had very poor resources already.”
Struggles amplified
The last thing they needed was the first thing they got: isolation.
For those battling depression, connection is key. Being around others, even if there’s no direct interaction, helps tether those with mental health issues to a society from which they feel unmoored.
“We try to encourage them as part of their treatment plans to attend group therapy sessions, to attend individual therapy sessions, to get out and socialize,” Still says. “Now, all of a sudden, because of this health crisis, they’re unable to do so. It can definitely exacerbate their mental health conditions.”
“I have folks dealing with depression who are getting triggered because they’re isolated and they’re having a hard time self-motivating,” says Donna Wilburn, a Las Vegas marriage and family therapist. “These are not the ones who can (say), ‘I’ll just go garden’ or ‘I’ll do something crafty,’ ” says Wilburn, who owns Dynamic Integrative Solutions counseling center. “Depression saps your motivation, so when you’re isolated, and there’s no work to force you out of the house, it’s really, really challenging.”
For those with anxiety, uncertainties about the spread of coronoavirus can amplify distress.
“The most trying thing is just hearing my clients’ anxieties and trying to help calm them down when the dissemination of the information — especially in the beginning — has been so murky,” Noonan says.
“I have anxious folks who are washing their hands OCD-style.” Wilburn says. “I literally have some who can’t sleep at night because of this. It’s really triggering a lot.”
And it could trigger more.
President Donald Trump sounded the alarm last week about a potentially dire mental health crisis when he said there would be “suicides by the thousands” should the economy continue to suffer.
While that may be a worst-case scenario, once again, Nevada seems particularly vulnerable.
The state had the 11th-highest suicide rate in the country according to a 2017 report, the most recent year for which data is available from the Department of Health and Human Service’s Office of Suicide Prevention. Suicide was the eighth leading cause of death for Nevadans, and the second leading cause of death for youth, ages 15-24. Nevada seniors over 65 have the fourth-highest suicide rate in the nation — almost double the national average.
People with mental illnesses that are linked to suicidal thoughts, such as depression, high levels of anxiety or more severe conditions, can be at higher risk, says Dr. Krystal Lewis, a clinical psychologist at the National Institute of Mental Health. “Unfortunately, there may be an increase in actual suicide attempts depending on how long this lasts.”
A new kind of therapy
The comfy office couch is gone.
“I have these ugly plastic chairs that I put in instead,” says Dr. Ann Childress, a Vegas-based psychiatrist and member of the Nevada Psychiatric Association. “I’ve moved my toys out of the waiting room. … so that we can minimize things that we needed to clean.”
Childress still is seeing clients in person, but now it’s one family at a time in the waiting room. And, like many in the profession, she is resorting to telemedicine and treating patients via phone.
Telemedicine was developed to serve rural communities with no doctors. Patients were required to visit a medical office, where they would consult with a physician in another city via teleconference.
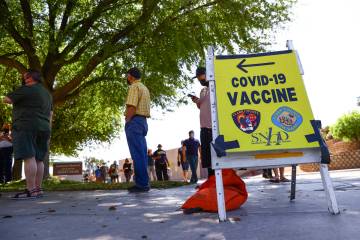
With the coronavirus outbreak, the federal government removed restrictions this month, allowing telemedicine to be covered by Medicare and Medicaid.
“It seems to be going pretty well,” says Still, after using telemedicine for a week and a half. Insurance companies his staff has contacted said they will reimburse such visits.
Local support groups are heading online as well.
While all the in-person meetings at NAMI (National Alliance of Mental Health) Southern Nevada have been canceled, executive director Trinh Dang says, beginning next week, some support groups will take place on Zoom.
“Even though, physically, we’re distancing ourselves,”,Dang says, “socially, emotionally, mentally, we’re hoping that we’ll be able to connect the community together again.”
Gonzalez says that online therapy sessions have helped.
“It’s a total change to go from the in-person to the digital world, but it’s amazing to have all the resources that we have right now,” she says. “I’ve heard so many people in meetings actually say, ‘This is my first Zoom meeting and I was hesitant about it. I didn’t think it was going to work.’ And then, at the end, they’re like, ‘I’m glad I did it, even if it’s not the same.’ I am physically alone in my mom’s apartment at the moment, but through these meetings, I know that I’m not alone.”
For some people, however, using technology creates a barrier to care.
“There’s a lot of people out there in the valley who aren’t able to connect to a mental health professional just because of the technology piece alone,” says Dr. Sheldon Jacobs, a Las Vegas mental health therapist and board member of NAMI Southern Nevada. “Some clinicians might get more creative or do some sessions over the phone, but how sufficient is that, not having that face-to-face?”
“It’s ending up being very heavily telephone (based), because a lot of people with mental illness are disabled and they don’t have enough money to buy a lot of data time,” says Dr. Joe Parks, vice president of practice improvement and medical director at the National Council for Behavioral Health. “They don’t have Wi-Fi hook-ups. A number of them don’t have computers. And often, people who have mental illness have cognitive problems that make it harder to use things like that. We tried to use Zoom, but we found that the patients really weren’t up to using it.”
“For some, the video platform is really uncomfortable,” says Wilburn, explaining why she still takes some in-person clients. “When I do have to see somebody face-to-face, we go through a whole sanitizing process. We’re able to keep our distance. But it’s hard with kids. How do you play with a kid six feet away? I don’t want to leave kids without help.”
How to cope?
“I think a lot of what I’m doing with children, and adults as well, is (asking), ‘OK, what is within our control?’ ” Krystal Lewis says. “For us, it’s having a schedule or structure,” such as working from home or doing online schoolwork. “It’s also integrating your general family time, time outside, exercise, making sure that there are these things that we know are good for our mental and physical health,” she adds. “This is what I can control right now: my day.”
Lewis and her peers have to navigate these turbulent emotional waters while coping with their own stress.
And, while therapists usually are able to balance patient needs, Wilburn says, “now everybody needs you.”
“I’m kind of caught between the pressure to help — so many people need my help right now — but I’m also trying to take care of my family, and (I’m) worried about not spreading this virus,” she says.
For mental health professionals who work in hospitals, there’s the heightened risk of being exposed to the coronavirus.
“I’m wearing personal protective equipment,” Still says. “I’m much more cautious in the hospital. … there’s some trepidation there. There are a lot of physicians who are afraid to work in hospitals knowing that we’re probably all getting exposed every day.
“I go home, and I can’t hug my family before I change and shower,” he continues. “Even with that, you never know what you’re bringing into the house. This has been a life-changer for everybody.”
So is it normal to feel anything but normal now?
“Feeling anxious, feeling uncertain, even feeling threatened is understandable,” says UNLV assistant professor of psychology Stephen D. Benning, who directs the university’s Psychophysiology of Emotion and Personality laboratory. “It is a realistic response to what’s happening.”
Unfortunately for some, that response might not end when social distancing does.
“There may be lingering echoes of this that ring for people for weeks or months afterward as they struggle to get back to a normal life,” Benning says. “This is the challenge we all face as a society after we return to normal: How do we get these people back in the swing with us?”
“I think that there’s a light at the end of the tunnel that isn’t a train,” Noonan says. “I’m hoping that we’re nearing it. It’s something that we’re going to get through.”
Contact Jason Bracelin at jbracelin@reviewjournal.com or 702-383-0476. Follow @JasonBracelin on Twitter.
MENTAL HEALTH RESOURCES
Center for Individual, Couple and Family Counseling
UNLV Campus
702-895-3106
Community Counseling Center
714 E. Sahara Ave., Ste. 103
702-369-8700
Mojave Mental Health
4000 E. Charleston Blvd., Ste. 230
702-968-4000
National Suicide Prevention Lifeline
1-800-273-8255
NAMI of Southern Nevada Help Line
702-310-5764