Hospice meets more than end-of-life needs
Richard, a spirited 90-year-old with a life-limiting disease, is graduating from hospice after a recent hip fracture. Who knew people could graduate from hospice without dying? There is much more to hospice care than just the last few days of a person’s life.
Dr. Brian Murphy, chief medical officer of Nathan Adelson Hospice, recently explained the true scope of hospice.
“Let’s talk about a nurse coming to your house at a minimum of every other week but it can be once, twice, more a week — nursing assistants who can help bathe you or do a little light housework, help get you out of bed, a social worker who will help you with getting your will together, financial papers or advanced directive, a chaplain who can work with your own spiritual counselor or be a spiritual counselor or just sit with you for a while,” he said. “The equipment that you need in your home is paid for — supplies, medications related to your illness — all paid for simply because you have Medicare. Who would turn that down?”
Why do so few people know about all the services hospice offers?
For many people, hospice is the ‘H’ word, and “People are afraid to talk about death,” said Karen Rubel, vice president for development for Nathan Adelson Hospice.
The hospice movement was started in the U.S. primarily by volunteers in the 1970s. The goal was to deliver quality comfort care to people facing life-limiting diseases. In 1983, Medicare created the hospice benefit. Hospice has evolved from a mainly volunteer staff into a professional interdisciplinary team focused on providing comfort, not curative care.
“People say all the time, ‘I wish I had known about this type of care sooner,’ ” said Brian Bertram, vice president of family-owned Infinity Hospice Care.
There are many misconceptions about hospice.
MYTH — Everyone who enters hospice dies in hospice
Because of the way hospice services have been utilized in the past, many people think that everyone who enters hospice is facing imminent death. Some, such as Richard, “graduate.”
Jerry Bolyard, regional executive director of Creekside Hospice, which has been in business in Las Vegas since 2001 and averages 370 daily services to patients with an in-patient care facility at 7230 Gagnier Blvd., explained how someone can graduate from hospice:
“Sometimes there is a debilitating event in somebody’s life (such as a broken hip, stroke or heart attack in a patient who has a life-limiting disease). We send in a nurse or a certified nursing assistant. What happens is you go from living alone and not being able to get your medications, not able to care for yourself, to now we’re making you a med-box. We’re making sure that you are clean (improve) and now you no longer qualify for hospice. I love the idea of an ‘I survived Creekside Hospice’ (graduation T-shirts).”
MYTH — There is only one hospice
Some people consider hospice a separate entity like the police or fire department. They don’t realize that there are approximately 50 hospice providers licensed by the Nevada Department of Health and Human Services in Clark County.
Nathan Adelson Hospice is the name most closely associated with hospice in Southern Nevada. Founded in 1978, it remains the largest not-for-profit hospice in the valley, caring for more than 400 patients a day.
MYTH — Hospice is only for the elderly
People of any age are eligible for hospice care as long as the criteria for hospice are met. Even children in a neonatal or pediatric intensive care unit can benefit from programs such as the Center for Compassionate Care Pediatric Program at Nathan Adelson Hospice.
MYTH — Hospice is expensive or a type of charity
Most private insurances include some kind of end-of-life care benefits that may limit the choice of hospice providers and services. Veterans are entitled to hospice benefits from the VA. Medicare Part A will pay 100 percent for Medicare-certified hospice programs.
“You have a right to use this service,” said Murphy.
MYTH — Hospice is only for the last few days of life
Even though Medicare requires a patient’s life expectancy to be six months or less, Medicare benefit periods were changed in the Balanced Budget Act of 1997 to include certifying and recertifying eligibility for two 90-day benefit periods followed by an unlimited number of 60-day periods. This allows for an indefinite extension of hospice care without a fear of losing coverage.
Medicare hospice benefits were meant to cover people who were going to die within six months, but Murphy knows that “doctors are notoriously poor at prognostications.”
According to Dr. Lisa Lyons, associate medical director of Infinity Hospice Care, the three-month certification period “is to really get a good look at the patient and see if their trajectory is down, or if it is up or just stable.”
MYTH — Only a doctor can refer someone to hospice
“You can pick up the phone and say, ‘I’d like to know if your services are right for my loved one, or myself (or neighbors, friends or out-of-town relatives),’ ” Murphy said.
Anyone can make an inquiry referral to hospice, but only a physician and a hospice medical doctor can certify that the patient has a terminal illness and likely has only six months or less to live. Sometimes a doctor will have a hard time deciding if a patient is ready for hospice.
Murphy has a simple question that he asks the doctor. “Would it surprise you if (the patient) will be gone in six months? If the doctor says no, then it’s time to call. If they say, ‘That would be a surprise,’ then it’s probably not the time to call.”
MYTH — Signing up for hospice is complicated and involves considerable paperwork
Medicare regulations entitle patients to choose their own hospice, as long as it is a Medicare-certified provider. With Medicare, patients have the right to change providers once during each benefit period if they are not satisfied with the service the hospice provides.
Paperwork includes an informed consent for hospice care, notice of privacy practices, notice of patient rights and responsibilities and a Medicare/Medicaid election that acknowledges assignment of the benefit to the hospice.
MYTH — Hospice care is available only in a hospice in-patient facility
“It’s not just a place that you go but a service that we provide that comes to you,” said Bertram. The majority of hospice care is provided in a patient’s home. This also can include assisted living and nursing homes.
“It’s a huge misconception that people have,” said Rubel. “That’s why they’re afraid to even ask (about hospice) because they don’t want to be displaced from wherever they call home.”
Murphy drives home this point by explaining, “We just travel with you so if you are at home, assisted living, nursing homes, into the hospital, out of the hospital, we just follow you the whole time.
“We have given hospice services in hotels (and) parks for homeless people, although we try to find them a place to live. Visitors end up accidentally dying here. We’ll go the Mirage or to Motel 6 if that’s where you are.”
In-patient hospice facilities are for short-term care to manage acute or complex symptoms or when a caregiver needs respite. Infinity Hospice Care, with offices in Las Vegas, Pahrump, Reno and Phoenix, is on schedule to open a new 12-bed in-patient facility this summer at 6330 S. Jones Blvd.
MYTH — Once PEOPLE choose hospice care, they have given up on life
For some people, knowing the “end game” gives them a new lease on life, time to get their affairs in order, make amends, say their goodbyes and enjoy the time they have left without trying to fight against their disease.
“We help find strategies; I like to call them hope strategies,” said Bertram. “Sometimes it’s not a realistic goal, and yet we don’t want to lose hope, and so if one of our hope strategies is (to walk and lose some weight), let’s get some physical therapy. It may work, it may not work, but here is a strategy. We want to help him focus on his quality of life.”
MYTH — Hospice care is mainly for cancer patients
According to the National Hospice and Palliative Care Organization, a professional self-reporting organization, in 2011, 62.3 percent of hospice admissions were for non-cancer diagnoses. These included dementia, heart disease, lung disease, stroke, coma, kidney disease, liver disease, HIV/AIDS and others.
MYTH — Hospice care doesn’t treat symptoms
The concept of hospice is a holistic approach to end-of-life care. If a person develops conditions such as bed sores, urinary tract infections, diarrhea or pain medication side effects, hospice doctors treat these conditions and others.
“Hospice works to alleviate suffering,” said Bertram. “When we think of suffering, we think of physical suffering first, yet the space that hospice really works well in is to alleviate the things that are causing us emotional stress or spiritual suffering. It’s the things that people are afraid of or don’t know what to ask or are thinking about that is causing them (to suffer).”
MYTH — Death is like it is portrayed on TV or in the movies
Most people have not witnessed someone else die. Murphy takes exception to the way death is portrayed on television.
“You’re talking, your eyes are open, and within five seconds your head tilts to the side and you die,” Murphy said. “We have a lot of people that are ready to go, but their bodies aren’t.”
Angela Ricker, R.N., director of patient services at Creekside Hospice, said, “I’ve had patients wake up and say, ‘Seriously? Really, God? I don’t know what you’re waiting for.’ ”
The goal of hospice is to ease the suffering of the families with compassion and empathy and to help them understand the dying process. Sometimes the last conversation a person has is with the hospice spiritual counselor.
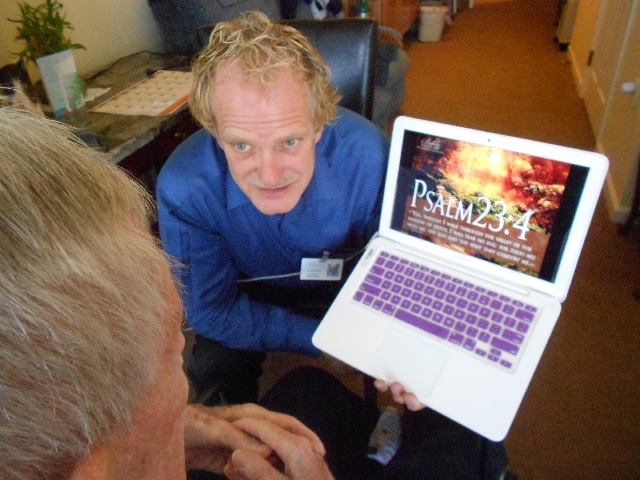
“People have preconceived ideas about dying,” said pastor Ron Magner, who turned to hospice counseling after 30 years of regular ministry. “The end of life is very spiritual.”
MYTH — Hospice gives people so many drugs that they die sooner
A common misconception about hospice care is that the patient will be overdosed with drugs in hospice and have a swifter death. Because people usually call hospice within the last days or hours of a person’s life, this myth has been perpetuated.
“They think we give you morphine and you die, which is clearly not true for everyone, and they’re afraid,” said Murphy. A recent study compared people in hospice who received morphine to patients who didn’t and there was no time difference in when they died.
MYTH — Hospice care shortens life
In the book, “The Best Care Possible” by Dr. Ira Byock, a national authority on hospice and palliative care, research is cited that analyzed Medicare data from 1998 to 2002 and compared survival rates of comparable groups of seriously ill patients who received and those who did not. Overall, in each group those who received hospice care lived an average of 29 days longer than those that did not. Those with congestive heart failure lived 81 days longer; lung cancer, 39 days; pancreatic cancer, 21 days.
When a new cancer drug extends life by one month and it is approved by the Federal Drug Administration, it is big news. “But no one goes on the news and says that you can have an extra month of your life with hospice,” said Murphy.
MYTH — Hospice health care workers are old and are finishing their professional careers working in hospice
Hospice is attracting more health care workers as the specialized field evolves. The University of Nevada School of Medicine offers a fellowship in hospice and palliative care medicine that is required to become board-certified in this new subspecialty of medicine.
Emily Brown, 30, a registered nurse for Infinity Hospice is a graduate of Nevada State College, and is working on her master’s degree at the University of Nevada, Las Vegas, to become a family nurse practioner.
“I love everything I do,” she said. After a personal experience with hospice in 2009, she experienced the caring and loving from hospice caregivers firsthand and knew that she wanted to make hospice nursing her career choice. “For me personally, it can be sad at times, but the overall picture is rewarding.”
Hospice help for caregivers
Services from hospice can help caregivers concentrate on “being the loved one” instead of the person giving care all day, every day.
Care giving “is difficult, time-consuming and physically and emotionally draining,” said Murphy. “We now have evidence to show that caregivers’ health declines and they have higher rates of PTSD (post traumatic stress disorder),” he said.
Many hospices have special programs that help caregivers reconnect with their loved ones. They use music, pictures and reminiscence techniques.
“Sometimes family members feel frustrated or guilty because they don’t know how to make a connection with their loved ones anymore — with dementia it changes who they are, and if we can just say, ‘Here’s a way you can be supported — we know it will improve the quality of the family unit,” said Bertram.
Hospice fulfills last wishes and mends fences.
Most people plan for the important events in their lives such as weddings and births, but the one inevitable event, death, is seldom discussed.
“Sometimes if we can bond with the family and build trust, we can teach the family that it is OK to say goodbye,” said Bertram. “Hospice provides clarity,” he said. “It lets the wishes of the patient be known sooner.”
Murphy said, “We are willing to get creative. Someone wanted to see their horse before they died. We brought the horse to the inpatient center. Honoring wishes even to the point of going to a casino one last time has always been a priority at Nathan Adelson,” said Murphy.
Choosing a hospice
Experts recommend talking to more than one hospice about the services they provide. Medicare pays a flat daily rate to hospice companies. Recipients are entitled to certain therapies that add a measure of quality of life and comfort, such as physical and speech therapy, as long as the therapy is not intended as a curative measure for the primary diagnosis. If a hospice doesn’t offer required certain services, it is wise to keep looking.
What is the hospice’s philosophy of care? Ask for examples of how they implement their philosophy into practice. What makes them different from other hospices? Does the hospice individualize its programs to fit the needs of the patient? Who are its doctors and nurses? Are the doctors board-certified in hospice and palliative care? How many full-time doctors and nurses do they employ? Are they available 24/7 and do they come to the home when they are needed in the middle of the night? Do they have an in-patient facility? Who is the contact person to call with questions?