Is this deadly fungus spreading outside of medical facilities?
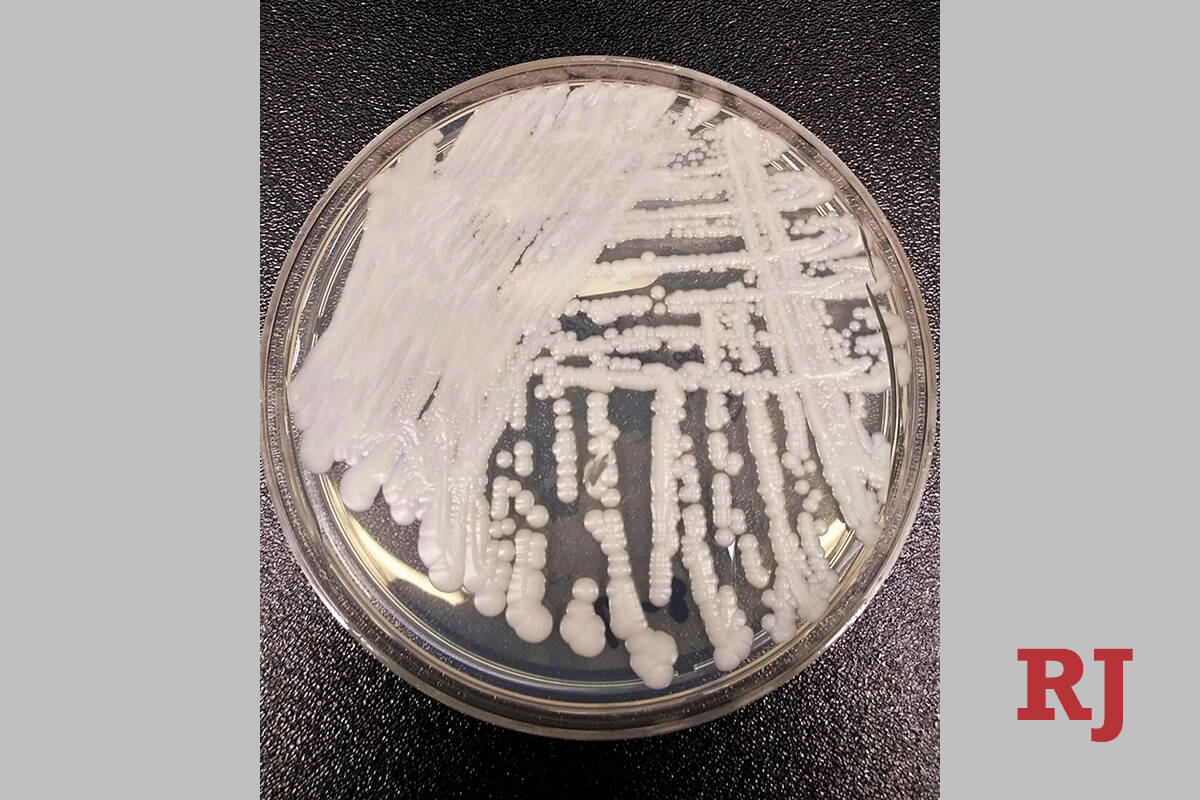
A small amount of evidence suggests that Candida auris — a potentially deadly fungus causing outbreaks in Southern Nevada hospitals and nursing facilities — is spreading outside of medical settings, health authorities said.
“There are no cases of C. auris that can provide compelling evidence of community spread at this time,” Mark Pandori, director of the Nevada State Public Health Laboratory at UNR’s school of medicine, said in an email Wednesday.
Five cases have been identified that suggest transmission may have occurred outside of a medical setting, but the evidence remains weak and more study is needed, he said. More than 1,200 total cases have been identified in Southern Nevada since August 2021.
The drug-resistant fungus can cause an invasive infection — in the bloodstream, heart or brain — which is deadly in one in three cases, according to the Centers for Disease Control and Prevention.
The most common symptoms of an invasive infection are fever and chills that don’t improve after antibiotic treatment for a suspected bacterial infection. The fungus is known to spread in hospitals and long-term care facilities from surfaces — such as a bed rail or piece of medical equipment — where it can survive for long periods of time.
People also can become colonized with the fungus, meaning it dwells in the folds of their skin, invisible to the eye, without making them ill.
The prevalance of C. auris in Southern Nevada’s wastewater suggests that the fungus is being shed by people outside of health care facilities, said Daniel Gerrity, principal research microbiologist for the Southern Nevada Water Authority. People shed pathogens through skin, saliva, feces and urine, which can enter the wastewater via toilets, sinks and shower drains. Water authority and UNLV researchers analyze waste water to help predict disease trends in the community.
No C. auris genetic material has been found in treated wastewater and there is no concern related to drinking water, Gerrity said.
Further study warranted
Last spring, in response to outbreaks in Southern Nevada, the Nevada Department of Health and Human Services in conjunction with the CDC expanded testing for the fungus. Some facilities are testing higher-risk patients, such as those with certain infections or wounds, upon admission.
There are instances of patients screened at a burn unit testing positive for C. auris despite no recent history of hospitalization, suggesting they might have been exposed outside of a medical setting, said Andrew Gorzalski, the molecular supervisor at the state lab.
Pandori described the current evidence of community spread as “concerning but not proof.”
“It is important that we look more closely to ascertain whether or not community spread is occurring,” he said.
The head of the CDC’s fungal disease branch agreed.
“We are still unclear as to whether community spread is an issue and it does warrant further study,” said Dr. Tom Chiller, head of the agency’s Mycotic Disease Branch.
“That being said, we do know that it is a pathogen that colonizes sick people in healthcare settings and does not seem to colonize healthy individuals readily, but that still needs to be confirmed,” Chiller said in an email.
Facilities not required to report cases
CDC data shows that in 2022, Nevada reported 384 invasive C. auris infections, which are also referred to as clinical cases. There were 2,377 total clinical cases reported across the U.S. in at least 27 states and the District of Columbia.
Nevada reported the highest number of clinical cases in the country, despite that it is one of 28 states not requiring facilities to report the new pathogen.
“Nevada is currently working through the process of adding C. auris to the list of reportable diseases,” Shannon Litz, a representative of the Nevada Department of Health and Human Services, said in an email. Meanwhile, there is “good compliance” among facilities with government recommendations to report cases, she said.
Prior to the outbreaks that began in Southern Nevada in August 2021, only one case had been identified in the state, in Northern Nevada in 2019, according to the state lab.
As of March 24, 723 colonization cases and 527 clinical cases have been identified in the state in at least 35 general acute-care hospitals, long-term care hospitals and skilled nursing facilities, according to the state health department.
Actively looking
One factor behind why Nevada has reported a high number of cases is that it is diligently looking for them, state health officials said.
“Through the coordinated response with the CDC, expanded testing has occurred and the state continues to work with facilities to conduct screenings for C. auris,” Litz said. “This increased identification helps facilities and the state’s public health infrastructure to manage and respond to cases.”
Many other states, she said, are not testing patients without symptoms.
Lawrence Muscarella, an authority on infectious diseases, said he isn’t convinced that Nevada necessarily had the most cases last year. The current CDC data on C. auris has not all been audited and validated, he said, and might be incomplete or inaccurate.
Furthermore, methods used by health care facilities to detect cases have not been standardized among the states or even within a single state, said Muscarella, who runs a Pennsylvania consulting company focused on health care safety.
As a result, “Nevada’s reporting the highest number of counted clinical cases last year does not necessarily mean Nevada had the highest number of actual clinical cases compared to the other states, or that its health care is poorer compared to other states,” he said in an email.
Muscarella said the number of deaths associated with the fungus would be a better metric for gauging the impact of C. auris than the number of cases.
Candida auris-associated deaths don’t get reported to the CDC and there is no national database that collects that information, CDC representative Katia Martinez said in an email.
There have been 103 deaths in Nevada in patients with Candida auris, Litz said. State officials have said that many of those who died had underlying health issues and that it can’t be determined whether C. auris was the cause of death.
In contrast, deaths in patients with COVID-19 who had underlying health conditions were counted as COVID-19 fatalities by the federal government. Not taking the same approach with C. auris, Muscarella said, “could undermine the CDC’s efforts to advise the public about the dangers of this fungus” and efforts to get funding to combat the disease.
For more coverage of Candida auris, visit lvrj.com/superbug.
Contact Mary Hynes at mhynes@reviewjournal.com or 702-383-0336. Follow @MaryHynes1 on Twitter.
For more coverage of the Candida auris outbreaks, visit lvrj.com/candidaauris or lvrj.com/superbug.