Clark County program slashes medical costs for homeless on Medicaid
Before he got off the streets and into his North Las Vegas apartment, the cost of Jeffrey Fikes’ monthly medical care was averaging $10,571 a month.
Now it’s running $2,423 a month.
That 77 percent decrease is due in large part to a first-of-its-kind public-private partnership between Clark County and Health Plan of Nevada that aims to reduce the load that Medicaid patients place on emergency rooms.
Rather than paying millions of dollars each year to diagnose and treat sick patients, the program provides participants with the housing, clothing and nourishment that will make them less likely to get extremely sick in the first place.
Started in August 2017, the Hospital to Home program has so far provided long-term supportive housing for 156 “super utilizers” of emergency room care, all of them homeless.
Officials with the county and Health Plan of Nevada say it has cut Medicaid costs for those participating by more than half.
‘Redefining health care’
“Number one, it’s kind of redefining health care,” said Ritchie Duplechien, who heads the program at Health Plan of Nevada.
“We’re looking at the whole person and not just the clinical aspects of how to save money on someone. We’re actually looking at what’s best for the people we’re serving.”
More than 14,000 people are expected to experience homelessness in Clark County at some point this year.
Of the 5,530 people counted during this year’s homeless census in January, 60 percent were unsheltered, meaning they were living in the tunnels under the Strip, in tents under overpasses or on vacant lots or in their cars.
Medical and mental health issues are two of the leading causes of homelessness, and those underlying conditions often result in repeat visits to the emergency room. Other times homeless individuals check in simply because they’re looking for reprieve from the heat or cold, a bed or a meal.
The most basic tests for a self-paying patient at University Medical Center’s emergency department cost $755 a visit, according to hospital officials.
But the state Department of Health and Human Services reimbursed the three managed care organizations operating in Nevada — Anthem Blue Cross Blue Shield, Health Plan of Nevada and SilverSummit — an average of $336.79 per patient for those on Medicaid, although rates can vary by location, age and gender.
Even so, those payments add up, and UnitedHealth Group Inc., America’s largest insurer and the parent company of Health Plan of Nevada, decided to try reducing its Medicaid expenses by investing in social interventions.
While Anthem Blue Cross and Shield and SilverSummit have provided Medicaid recipients with similar wraparound services, Health Plan of Nevada is the only managed care organization to enter in a public-private partnership with the county.
“There has been a shift over the last five to 10 years to really examine how social determinants affect the lack of housing, the lack of food insecurity, stable employment, companionship,” DuAne Young, deputy administrator on medical programs for Nevada Medicaid, said of the reasoning behind the partnership.
“Being able to have someone around to help care for them and housing is a major piece to them and if a person is not housed, and they have a wound, they’re not going to be able to heal properly on the streets.”
It’s something Jill Buckley, executive director of clinical redesign at UnitedHealth, also emphasizes.
“I mean, where do you plug your oxygen in when you’re out on the corner of Second and Main?” she asked.
Providing a ‘new reference point’
The Hospital to Home program has made a huge difference for Fikes, 41.
After a five-year battle with depression following a failed relationship and an arrest for driving under the influence, he quit his job, lost his apartment and lived in his car. He attempted suicide in 2016 while staying at a friend’s house by swallowing an assortment of prescription pills.
Ten days later, he woke up and couldn’t tie his shoes. The long period he spent unconscious on the ground had caused some of his muscles to “die” from lack of oxygen. His family was told he wouldn’t survive, and doctors later came close to amputating both of his arms and one leg.
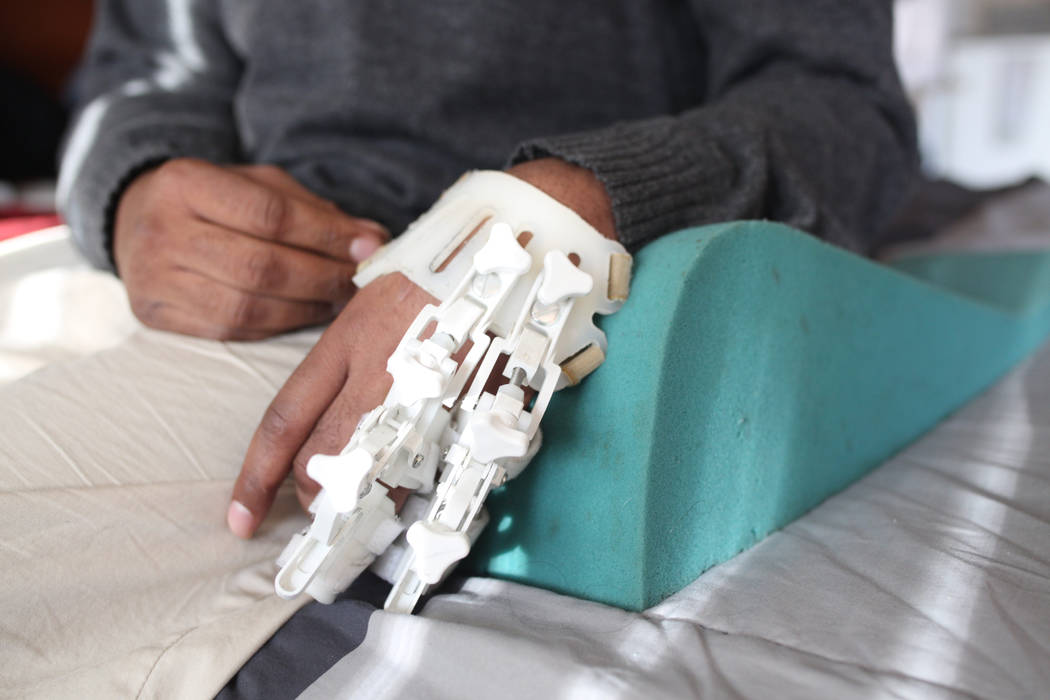
Fikes subsequently had multiple surgeries over three months to eliminate blood clots, save a kidney and remove dead tissue in his arms. He also developed compartment syndrome, a painful chronic condition that occurs when pressure within the muscles builds to dangerous levels, decreasing blood flow and, in some cases, preventing the sufferer from being able to move.
That triggered an associated condition, called Volkmann contracture, which causes his left hand and fingers to curl in a claw-like ball.
Fikes was in a rehabilitation hospital, with no home to return to, when he was referred to the Hospital to Home program through Health Plan of Nevada. The program placed him into his studio apartment in November 2017.
Health coaches for Health Plan of Nevada provided a long-term health plan to monitor his wellness. They also provided transportation to doctor’s appointments and the grocery store and helped him apply for benefits.
“Instead of checking them out right before they go into the waterfall, we’re going to check them out before they fall into the stream,” Duplechien said. “Sometimes, it’s as simple as having a refrigerator to put insulin in for their diabetes.”
For Fikes, having a home was “the reference point” he needed.
“It’s the quality of life, being at ease with my condition,” he said. “When you’re out on whatever street, you’re worrying about everything.”
Through HELP of Southern Nevada, the county pays $725 a month for Fikes’ rent and he’s in the process of applying for disability in hopes that he can leave the program and become self sufficient.
60 beds for the medically fragile
For the current fiscal year, Health Plan of Nevada has paid $308,904 for case management services and the county contributed $930,884 for housing assistance, according to county officials.
That public-private partnership with Health Plan of Nevada is the first of its kind in the three cities that have tested the program, which is part of a UnitedHealth initiative that it calls MyConnections. The Clark County program is the first to use a scattered housing model and supports 60 beds for the medically fragile throughout the Las Vegas Valley.
The partnership is laying the groundwork for an approach to treatment that “creates a service array and capacity that the county can’t do in silos,” Assistant County Manager Kevin Schiller said.
“It created the opportunity for us to work together because their client is our client, and we’re going to be able to grow this much larger because of the ability to have a joint-funded model,” he said. “With managed care, we can kind of focus on a win-win with the perspective of we want to give the clients the best care we can.”
But key is picking the right patients that will be successful in the program, UnitedHealth officials say.
Health Plan of Nevada has focused on identifying “super utilizers” — patients whose medical spending exceeds $50,000 a year.
There may be opportunities to expand and refine the approach next year.
On Jan. 1, a new state bill passed this year will provide Medicaid reimbursement to local governments or nonprofits that provide case management services for patients.
Senate Bill 425 allows Medicaid to pay for those items, which will pave the way for social service providers to expand their reach, according to Young, the state Medicaid administrator.
“Providers will be able to transition their funds into housing,” Young said.
“It’s going to take a while, so our hope over the next couple years is to really introduce a continuum of care, and we have Medicaid funds to supplement the resources and the supports of getting a person into housing and keeping them into housing.”
A ray of hope for others
As for UnitedHealth, its Las Vegas model is considered a success and is likely to be a template for other markets around the U.S.
UnitedHealth has invested $400 million in affordable housing and hopes to house 350 homeless Medicaid patients whose total annual health-care spending exceeds $17 million by early next year. It also plans to expand the national initiative to 30 new markets.
Some homeless individuals living in dire medical circumstances on Las Vegas streets said they hadn’t heard of the new program.
Nick Lerma, 39, who lives at the city of Las Vegas’ Courtyard Homeless Resource Center on Foremaster Lane, considers it a good option for him. Lerma, a Medicaid recipient, said he lost his housing voucher two years ago after he missed an appointment due to being hospitalized.
Lerma suffers from a rare bone infection called osteomyelitis that forced him to have his legs amputated and left him confined to a wheelchair. With his condition, even the smallest cuts can cause Gangrene.
“Sometimes, I can’t concentrate on my homelessness; there’s times that I spend three months in the hospital,” he said. “I just come right back to the Courtyard.”
Contact Briana Erickson at berickson@reviewjournal.com or 702-387-5244. Follow @ByBrianaE on Twitter.