Reinfections account for a growing percentage of COVID-19 cases
Reinfections account for about 9 percent of new COVID-19 cases reported in Nevada, according to state data, a growing number blamed in part on easily transmissible variants.
This is triple the overall rate of 3 percent of cases since the beginning of the pandemic, according to data from the Nevada Department of Health and Human Services.
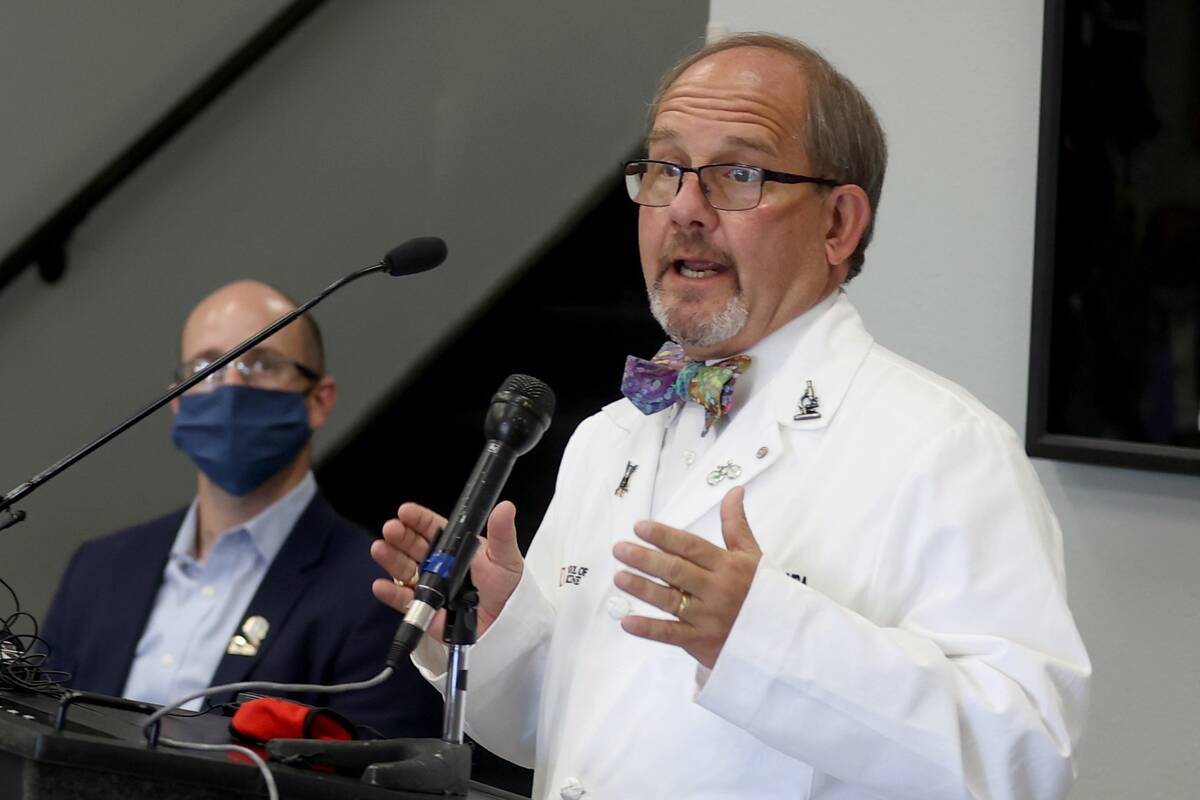
“Since January, reinfections are a greater proportion of total infections,” said Dr. Marc Kahn, dean of the Kirk Kerkorian School of Medicine at UNLV. “And most of that is because of the infectivity of both omicron and the BA.2 variant.”
Before the omicron surge this winter, the combination of vaccination and prior infection appeared to make an individual almost bullet-proof to reinfection, Kahn said. However, the omicron variant, whose technical name is BA.1, along with omicron descendant BA.2, have shown a greater ability to evade the immunity conferred by vaccination or prior infection.
The current vaccines were formulated to protect against the original strain of coronavirus, and are far less effective against these newer variants, said Mark Pandori, director of the Nevada State Public Health Laboratory at University of Nevada, Reno. Fortunately, the messenger RNA vaccines by Pfizer-BioNTech and Moderna could be retooled relatively quickly to respond to new variants.
Neither is the natural immunity triggered by an infection of an earlier strain as effective against the new strains.
Immunity also wanes over time, particularly with the coronavirus family of viruses, Pandori said. Too, people are letting down their guard against the virus by not wearing masks and no longer social distancing.
As a result of this combination, “The rate of reinfection has really skyrocketed,” he said.
For some people, this has meant getting reinfected not just once but twice, according to emerging data, Pandori said.
Reinfections underestimated
The threat of reinfection convinced Summerlin retiree Mike Deming to get both vaccinated and boosted.
Deming was sick for more than a week in December 2020 with a bad cough, headache and exhaustion. His wife, who was experiencing similar symptoms, tested positive for COVID-19. His PCR test came back as inconclusive, but his doctor with the VA Southern Nevada Healthcare System expressed certainty that he, too, had gotten the coronavirus.
For several days, “I couldn’t get out of bed, I had no energy,” the 74-year-old former construction manager said.
“I decided ‘I’m not gonna go through this again,’” he said, and later got two doses of Pfizer vaccine and a booster shot.
Then in December of last year, Deming tested positive for COVID-19 using an at-home rapid test. This time, his symptoms were milder and lasted only a few days, he said.
The growing use of rapid at-home tests is likely resulting in an underestimation of reinfections, since these results are not reported and aren’t included in state data, Kahn said.
“But the good news is that with reinfection, it is for the most part, a much, much milder disease,” the UNLV dean said.
The not-so-good news in some respects is that many authorities believe that the coronavirus will begin to behave more like a seasonal flu – which though resulting in milder cases, may require an annual shot to help keep infection or reinfection at bay.
Rapid reinfection reported
Coronavirus reinfections account for 22,122 out of 714,925 total reported cases in Nevada, or about 3 percent, Shannon Litz, a state health department representative, said in an email. For March, the rate was 9 percent, or 397 out of 4,396 total cases.
The Centers for Disease Control and Prevention did not respond to a request for information on U.S. reinfection rates. The agency’s website states “CDC is using a range of data sources to assess how often reinfections occur, who is most at risk for reinfection, and the risk of reinfection when there is community spread of Omicron or other virus variants.”
Since mid-December 2020 when vaccines became available, vaccinated people in Nevada had 9,131 reported reinfections, and unvaccinated people had 12,701 reinfections. Another 290 reinfections occurred before vaccines became available.
Data was unavailable on reinfections in people both vaccinated and boosted.
As of April 7, there had been 73 deaths from reinfection in the state compared with 9,107 from original infection. Another 1,072 deaths need additional investigation, Litz said.
The average number of days between the original case and reinfection has been 382.
A case is considered a reinfection when a person who has tested positive for COVID-19 and recovered tests positive again at least 90 days after the original test. A case also is considered a reinfection when sequencing, a process of genetic analysis done in a laboratory, determines that a person is infected with a different strain than the original infection.
There likely are unreported cases of reinfection that occur prior to the 90-day threshold adopted by the Centers for Disease Control and Prevention and that are not detected through sequencing, which is done on only a sampling of positive tests, Pandori said.
Sequencing at Pandori’s lab confirmed that a 31-year-old man tested positive in September of last year for a second infection just 22 days after testing positive for a different strain.
Kahn said the unvaccinated as well as those people with compromised immune systems generally are more susceptible to reinfection.
The same methods used to prevent infection also help to prevent reinfection, he said: getting vaccinated and boosted, masking, and practicing good hygiene such as hand-washing.
Contact Mary Hynes at mhynes@reviewjournal.com or 702-383-0336. Follow @MaryHynes1 on Twitter.